Scottish Welfare Fund news - October 2023
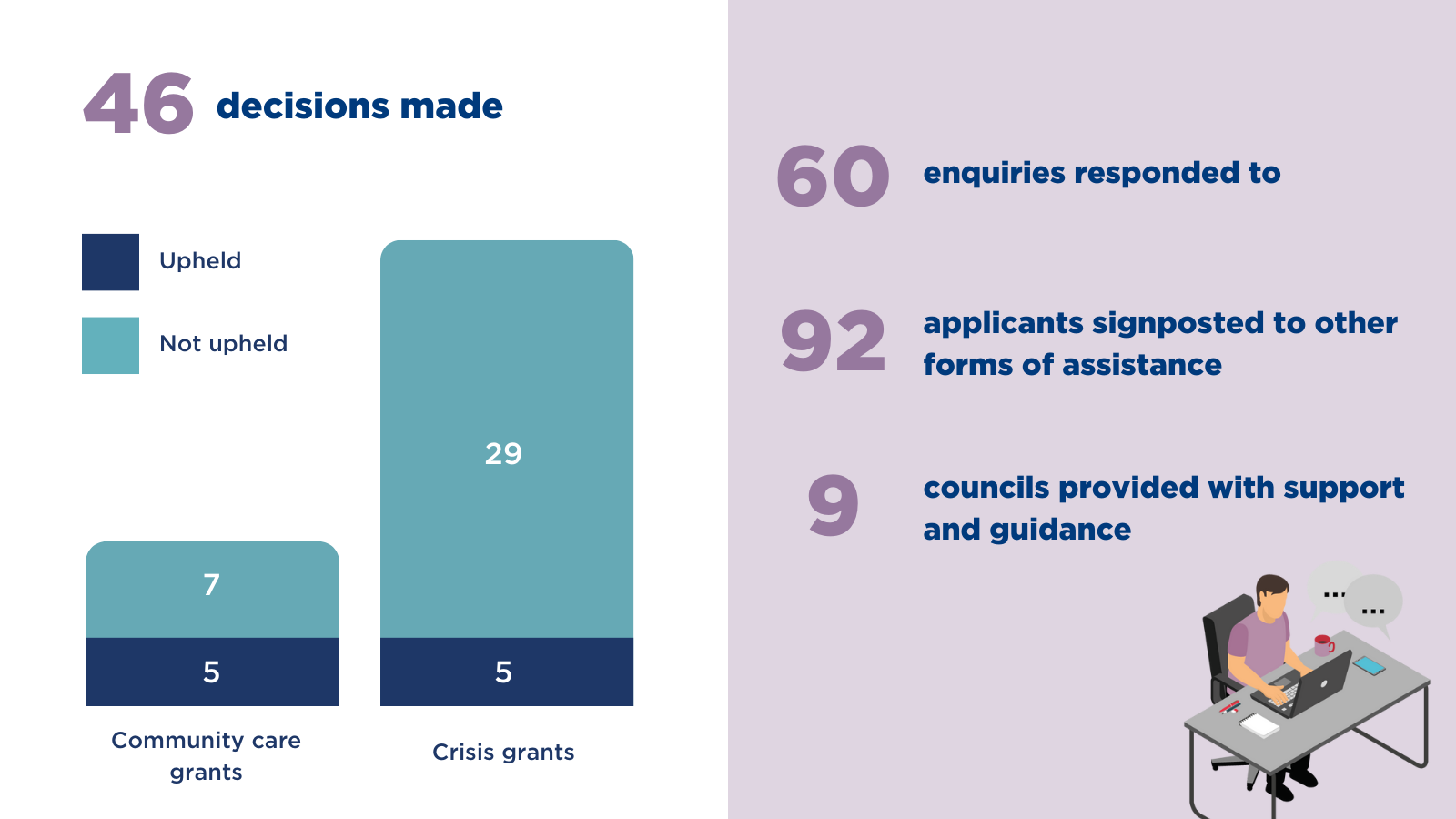
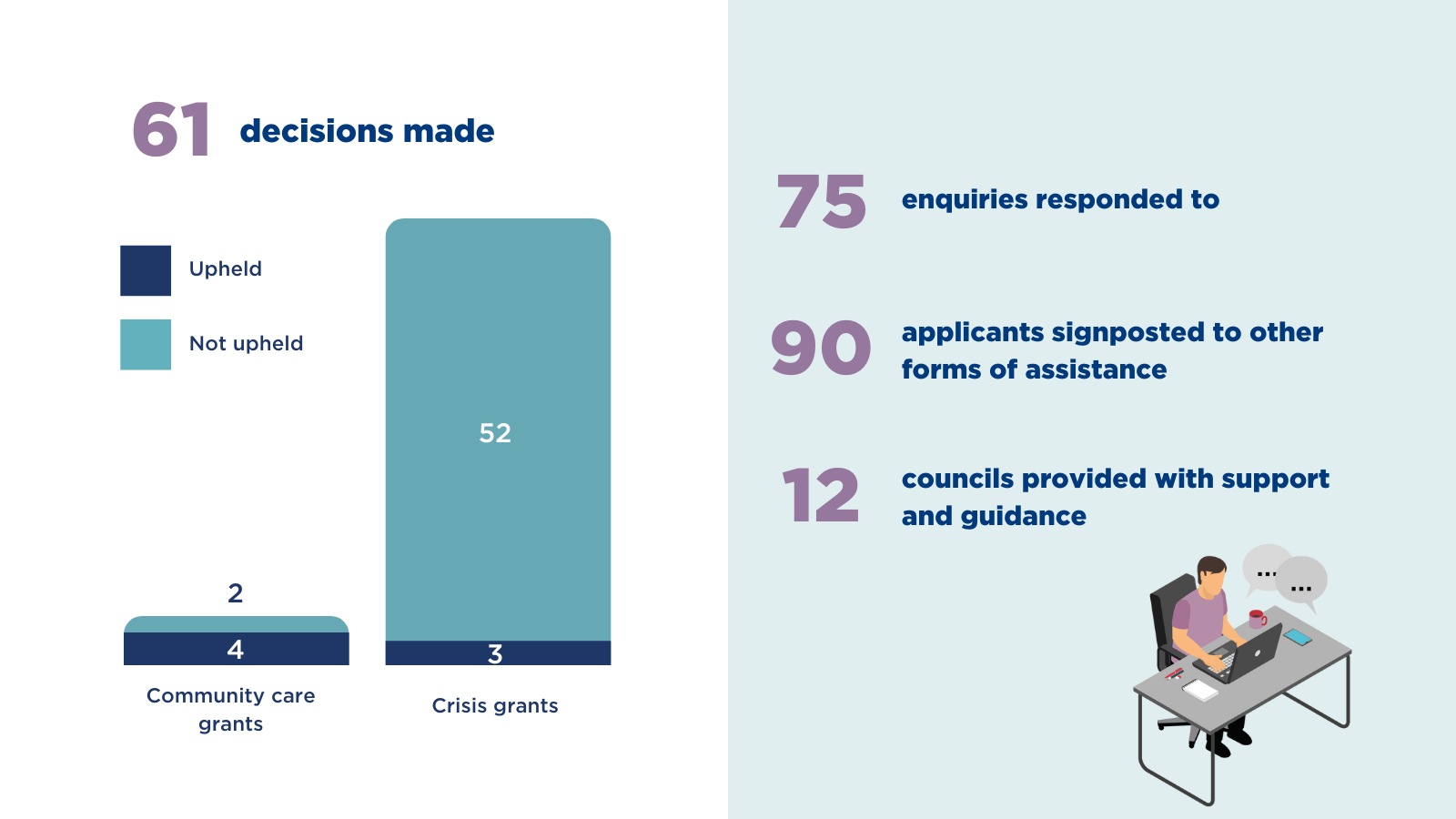
Last month we:
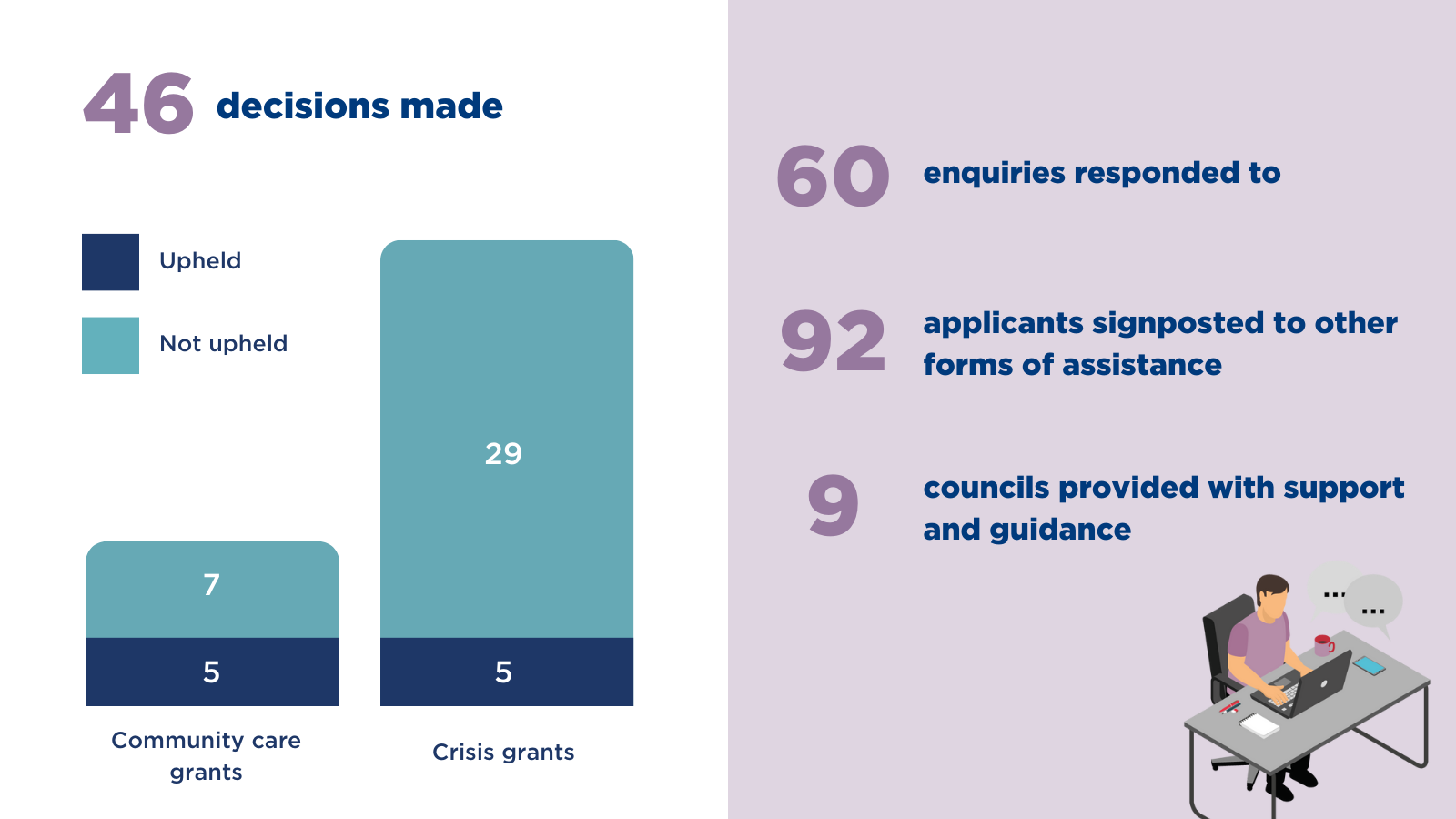
Last month we:
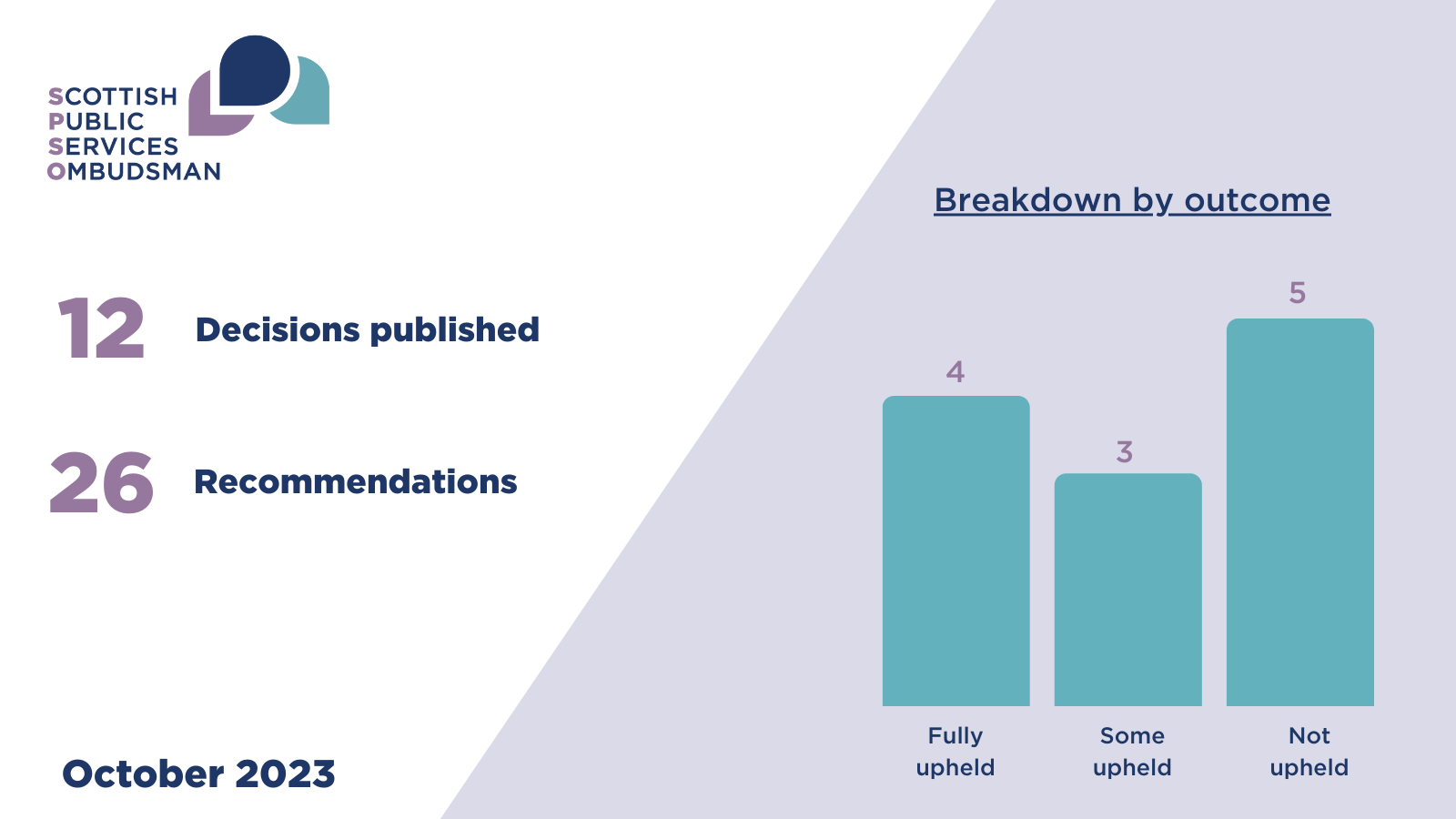
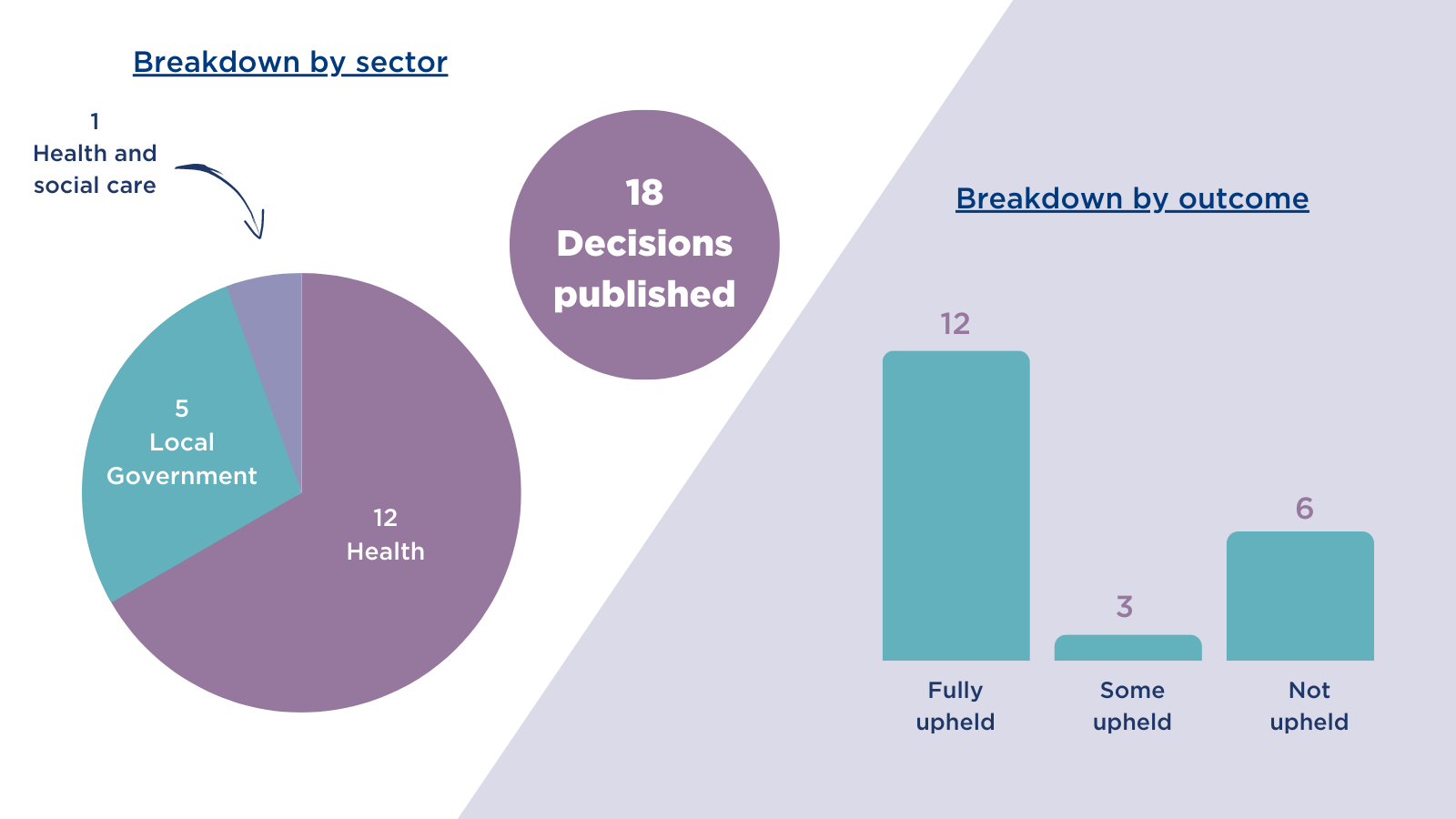
This month the Ombudsman’s findings highlight the importance of following good complaints handling procedures and having mechanisms in place to learn from complaints.
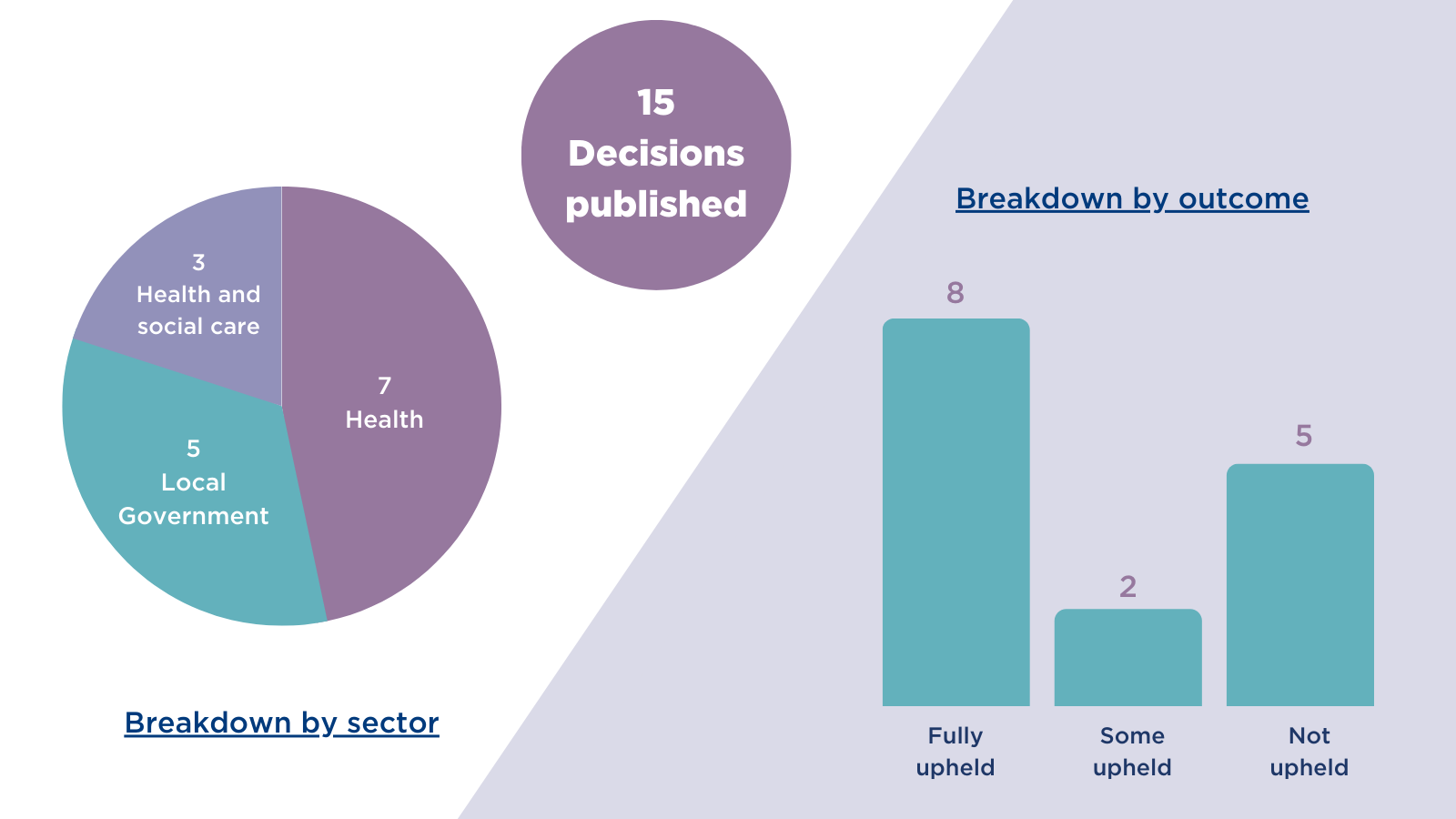
This month the Ombudsman’s findings highlight the importance of public bodies managing service user expectations, ensuring all involved have a clear understanding of the service being provided
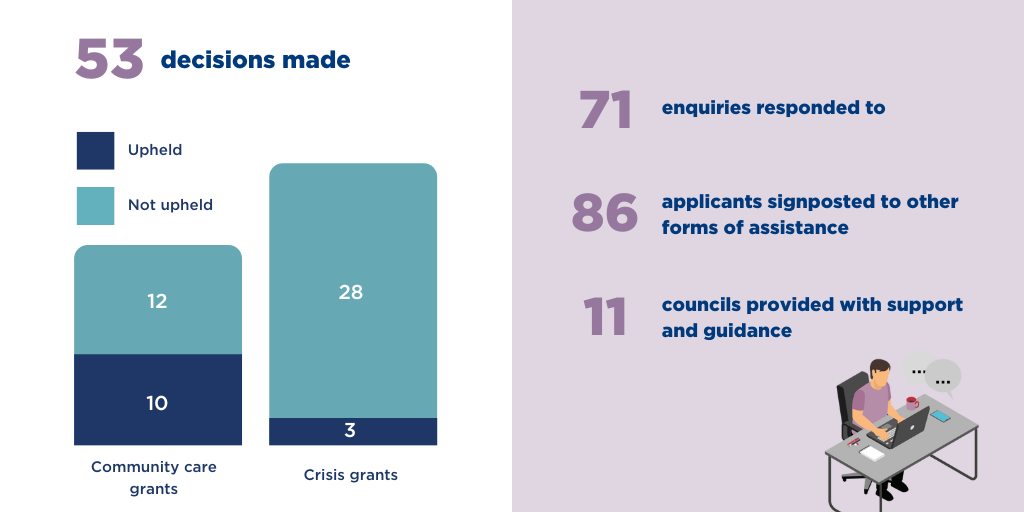
Last month we:

Ticket registration is now open for SPSO Conference 2023: Supporting Good Complaints Handling in a Changing World - take advantage of our early bird discount for a limited time only!
Last month we:
This month the Ombudsman’s findings highlight the importance of public bodies following guidance, policies and procedures, which are often in place to protect staff and service users.