Scottish Welfare Fund update - August 2025
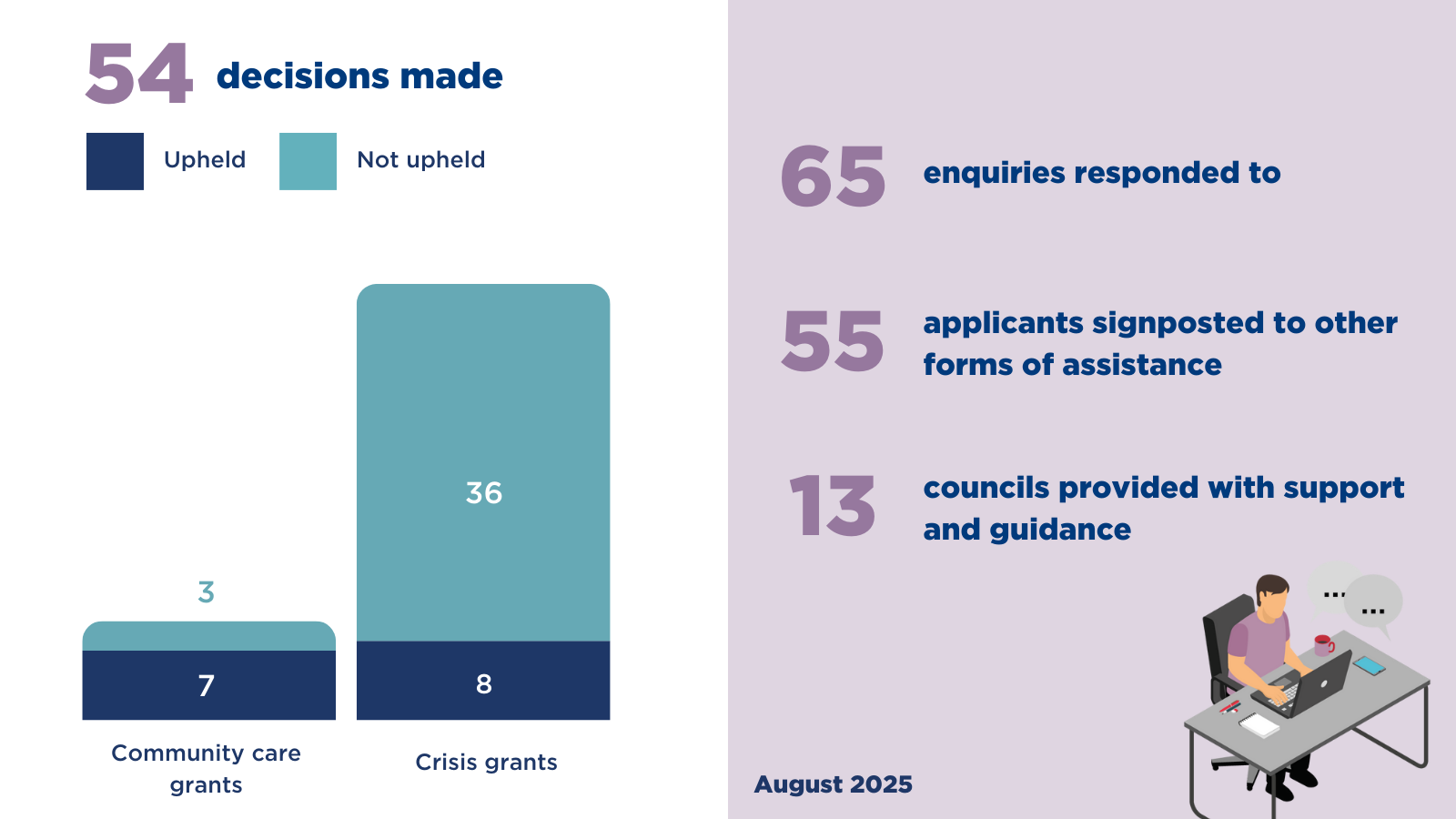
During July we
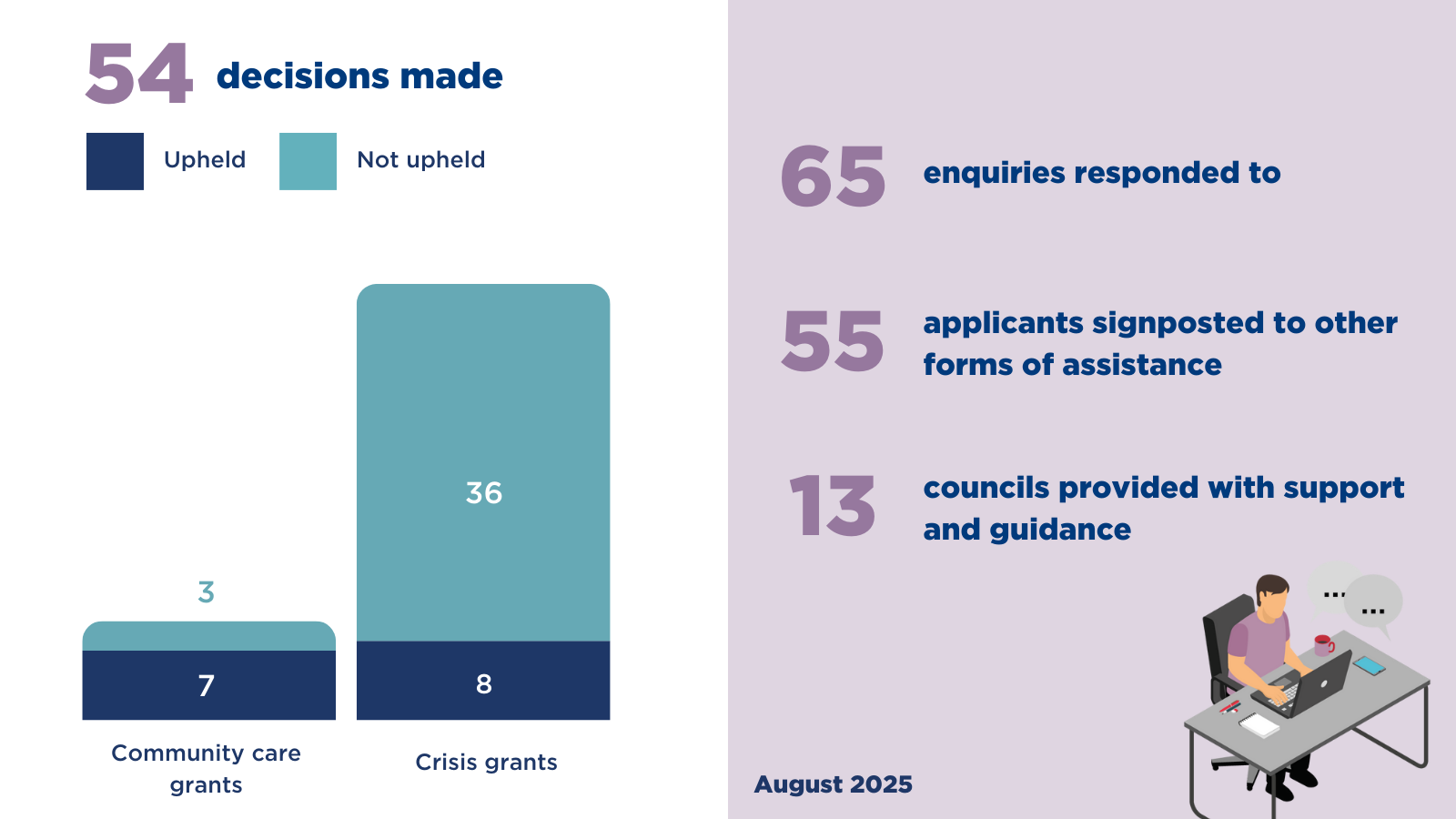
During July we
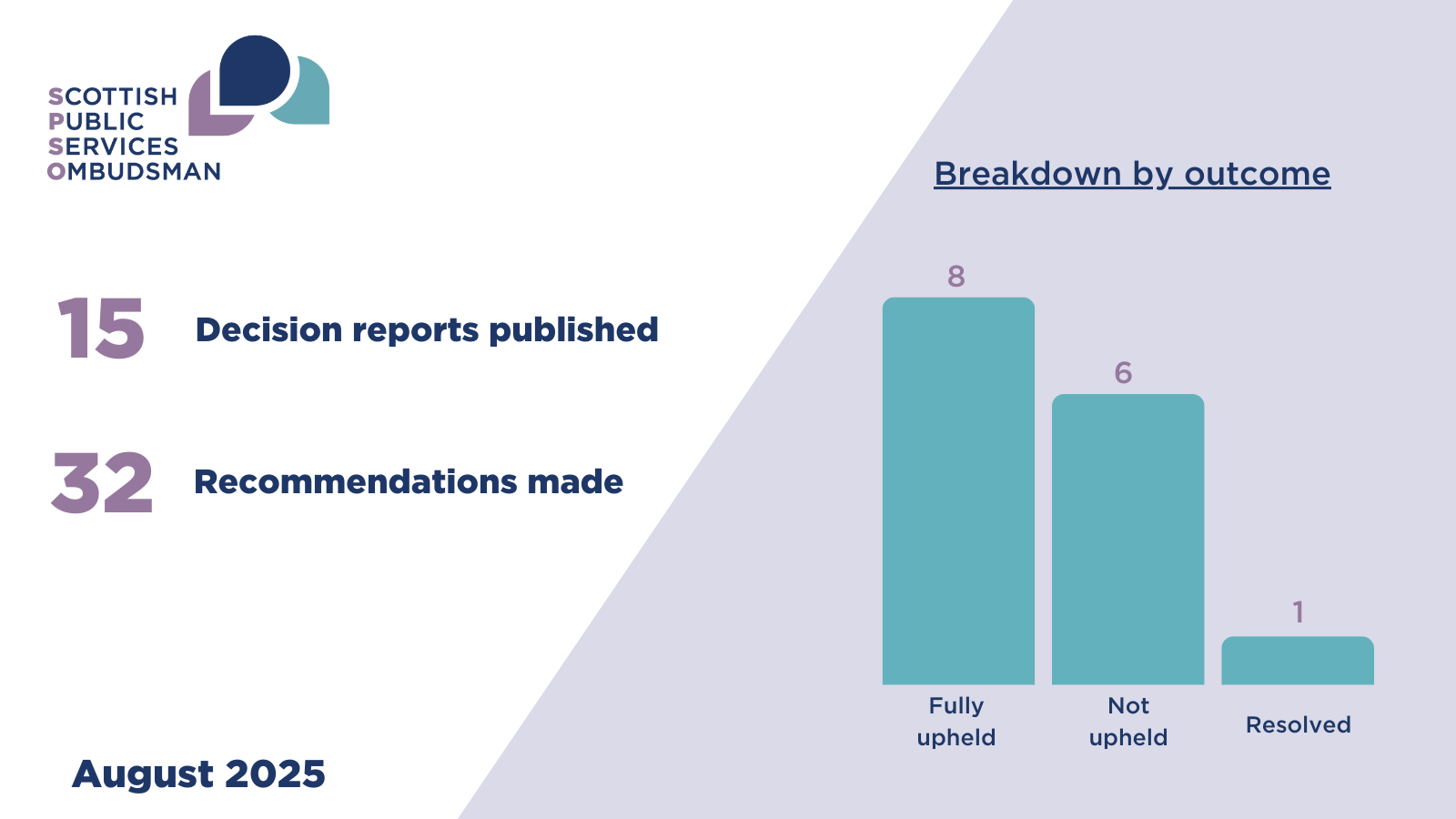
In this month’s edition of the Ombudsman’s findings, we highlight our recent investigation report.
The complainant (C) complained to me about the standard of nursing care and treatment provided to their late spouse (A) by Borders NHS Board (the Board). In particular, C was concerned about how nursing staff cared for and treated A.
A was cognitively impaired and suffered from terminal prostate cancer with cancer in their bones. Following a period of delirium, A was admitted to hospital for pain management; they had complex pain needs including neuropathic pain. A also had a tendency to wander.
C complained to me that A’s pain, and their tendency to wander, was not managed in a reasonable way and that nursing staff actions, including communication towards C, was unreasonable.
The Board said in their response to C that, overall, they considered A’s care was appropriate; A had their pain assessed daily and only required additional pain relief on two occasions. A’s tendency to wander had also been managed by following specialist advice. However, there were a number of shortcomings in communication with C for which the Board apologised.
During my investigation I sought independent advice from a registered nurse. Having considered and accepted the advice I received, I found that:
Taking all of the above into account, I upheld C’s complaint about the standard of nursing care and treatment provided to A.
Having considered the Board’s complaint file and the evidence from the clinical records, I also found the Board’s complaint handling was unreasonable in that there was a failure to ensure the complaint response was accurate and substantiated by the clinical records. The Board also failed to provide a clear and full complaint response.
What we are asking Borders NHS Board to do for the complainant:
| Rec number. | What we found | What the organisation should do | What we need to see |
|---|---|---|---|
| 1. |
Under complaint (a) I found that the standard of nursing care and treatment was unreasonable in that the Board failed to:
Under complaint point (b) I found that complaint handling was unreasonable in that there was a failure to:
|
Apologise to C for the failings identified in this investigation in relation to the standard of nursing care and treatment and complaint handling. The apology should meet the standards set out in the SPSO guidelines on apology available at www.spso.org.uk/meaningful-apologies. |
A copy or record of the apology. By: 22 September 2025 |
We are asking Borders NHS Board to improve the way they do things:
| Rec number. | What we found | Outcome needed | What we need to see |
|---|---|---|---|
| 2. |
Under complaint (a) I found that the standard of nursing care and treatment was unreasonable in that the Board failed to:
|
Patients who are cognitively impaired and in pain should be assessed by the appropriate tool, and receive adequate pain relief. Patients should receive person centred care and for those with cognitive impairment, information provided by carers and/or family members should be taken into account to ensure person centred care planning. Staff should take into account any specialised advice provided. If a decision is made not to act on it, the reason for this should be documented. Documentation and record keeping should meet the required standards and policy. |
Evidence that the findings of my investigation have been fed back to the staff involved, in a supportive manner, for reflection and learning. Evidence staff are competent in the use of the relevant pain assessment tools and take into account relevant guidance and specialist advice. For example, by the carrying out of a ward audit, and identifying and addressing training needs. Evidence that person centred care documentation meets the required standard. For example, by the carrying out of a ward audit, and identifying and addressing training needs. By: 20 November 2025 |
We are asking Borders NHS Board to improve their complaints handling:
| Rec number. | What we found | Outcome needed | What we need to see |
|---|---|---|---|
| 3. |
Under complaint point (b) I found that complaint handling was unreasonable in that there was a failure to:
|
Complaints should be investigated fairly and fully and in line with the requirements of the NHS model complaints procedures. Complaint responses should be accurate, complete and address all the points raised in line with the NHS model complaints handling procedure. We offer SPSO accredited Complaints Handling training. Details and registration forms for our online self-guided Good Complaints Handling course (Stage 1) and our online trainer-led Complaints Investigation Skills course (Stage 2) are available at https://www.spso.org.uk/training-courses. |
Evidence that the findings of my investigation have been fed back to the staff involved, in a supportive manner, for reflection and learning. By: 22 September 2025 |
Borders NHS Board told us they had already taken action to fix the problem. We will ask them for evidence that this has happened:
| Complaint number | What we found | What the organisation say they have done | What we need to see |
|---|---|---|---|
| (a) |
Under complaint (a) I found that the standard of nursing care and treatment was unreasonable in that the Board failed to:
|
Training for nursing staff on detention orders under the relevant legislation. |
Evidence training occurred. By: 22 September 2025 |
 The Scottish Public Services Ombudsman (SPSO) has published its updated Statement of Complaints Handling Principles, approved by the Scottish Parliament in June 2025.
The Scottish Public Services Ombudsman (SPSO) has published its updated Statement of Complaints Handling Principles, approved by the Scottish Parliament in June 2025.
Your feedback is important to us.
The complainant (C) complained to my office about the nursing care and treatment given to their late parent (A) at home and in hospital (acute care) by Lothian NHS Board (the Board). A was an adult with multiple sclerosis (an autoimmune condition that affects the brain and/or spinal cord). Due to progression of the condition A was doubly incontinent, immobile, and unable to eat or drink independently. A required assistance daily from carers and weekly from district nurses.
A developed pressure damage to their skin whilst in the community, and they were later admitted to hospital with sepsis (overwhelming infection). A was discharged home and readmitted within a short period of time. They died shortly after their readmission to hospital.
C raised concerns that A did not receive appropriate treatment at home from the district nurses, and specifically that, pressure damage was not treated appropriately. C also raised concerns about the standard of acute nursing care specifically in relation to; pressure damage, nutrition, basic care, and record keeping.
The Board said that the district nursing team considered that they had provided reasonable nursing care to A whilst they were at home. The Board also said, acute nursing staff were made aware of A’s needs and were concerned about the integrity of A’s skin. The Board highlighted that regular drinks were offered to A, however, A declined these on occasions. It was noted that some documentation was not present in the medical records. An action plan was agreed to make improvements in staff awareness, completion of documentation, and the importance of charts.
During my investigation I sought independent clinical advice from a registered nurse with experience in both community and acute care settings and with particular knowledge of the management and treatment of pressure damage.
Having considered and accepted the advice I received I found that:
There was evidence of significant omissions in the care provided by the district nursing team including
There was evidence of significant omissions in the acute care provided by the Board including
Taking all of the findings above into account, I upheld C’s complaints.
What we are asking the Board to do for C:
| Rec number. | What we found | What the organisation should do | What we need to see |
|---|---|---|---|
| 1. |
Under complaint point (a) I found that the district nursing care and treatment was unreasonable. Under complaint point (b) I found that the nursing care and treatment given to A in hospital during two admissions was unreasonable. |
Apologise to C for the failures identified in this report. The apology should meet the standards set out in the SPSO guidelines on apology available at www.spso.org.uk/meaningful-apologies. |
A copy or record of the apology. By: 25 August 2025 |
We are asking Lothian NHS Board - Acute Services Division to improve the way they do things:
| Rec number. | What we found | What the organisation should do | What we need to see |
|---|---|---|---|
| 2. |
Under complaint point (a) I found that the district nursing team failed to
|
Patients receiving district nursing care in the community should be appropriately assessed and have appropriate care plans in place that are regularly reviewed and updated. |
Evidence that the findings of my investigation have been fed back to the district nursing team involved in a supportive manner for reflection and learning. By: 25 August 2025 Evidence the Board have taken action to ensure all staff are proficient in completing risk assessments (including Waterlow) and developing person-centred care plans. By: 24 November 2025 Evidence an independent audit of patients within the district nursing care has been completed by an independent person external to the Board with the appropriate level of expertise and experience. The purpose of the audit should be to ensure that district nursing care has been appropriately undertaken. In particular that appropriate risk assessments (including Waterlow) are in place, along with a person-centred care plan and where appropriate a wound care chart. If gaps are identified, evidence that action has been taken to rectify the situation in each case. Progress update by: 24 November 2025 Completed audit by: 23 January 2026 |
| 3. |
Under complaint point (a) I found that the district nursing team failed to plan two person visits to A after it was identified this was required to complete basic nursing care, particularly skin checks. Under complaint point (a) I found that the district nursing team relied on A to report on their own skin condition when unable to assess their own skin. |
Patients receiving district nursing care should be given basic nursing care with regular checks, such as skin checks, as required. Patients should receive safe and appropriate care from an adequate number of district nursing staff and in line with their assessed needs. Patients who are frail, immobile, experiencing deteriorating health, and who are unable to visually check, should not be expected to report on their own well-being or condition (i.e. skin health) in lieu of appropriate checks by a clinician. |
Evidence that the findings of my investigation have been fed back to the district nursing team involved in a supportive manner for reflection and learning. Evidence an independent audit has been completed as detailed in recommendation 2. Progress update by: 24 November 2025 Completed audit by: 23 January 2026 |
| 4. |
Under complaint point (b) I found that the hospital nursing team failed to
|
Patients who are admitted to hospital should be appropriately assessed and have a person-centred care plan in place. These should be reviewed regularly. |
Evidence that the findings of my investigation have been fed back to the relevant involved in a supportive manner for reflection and learning. By: 25 August 2025 Evidence an independent audit of inpatient nursing care, particularly in relation to the carrying out of nursing assessments and completion of patient paperwork/documentation. This should be carried out by a person independent to the Board with the appropriate level of expertise and experience. The purpose of the audit would be to ensure that appropriate nursing assessment and documentation is completed within the correct timescales, and that particular consideration has been given to ensure wound charts are completed as required by the Vale of Leven Enquiry recommendations 2014. Progress update by: 24 November 2025 Completed audit by: 23 January 2026 |
| 5. |
Under complaint point (b) I found that there was a delay in making appropriate referrals for specialist review of A. Specifically there was
|
Patients who require specialist review/input into their care should have referrals made without delay. |
Evidence that the findings of my investigation have been fed back to the district nursing team involved in a supportive manner for reflection and learning. Evidence that the Board have robust referral pathways in place for:
By: 23 September 2025 |
| 6. |
Under complaint point (b) I found that care and treatment provided by nursing staff was unreasonable, particularly
|
Patients who are admitted to hospital should receive reasonable basic nursing care to meet their needs. Patients with skin damage/pressure damage should receive care and treatment using appropriate and correct products that are safe for them and their condition. Patients with, or at risk of, pressure damage should receive reasonable nursing care and treatment including regular repositioning. When they are reluctant to be repositioned, they should be offered the use of turn assist equipment to help. Patients who have been admitted to hospital should have their basic nutritional and hydration needs met, particularly when, they are unable to meet their own needs independently due to their medical condition. Patients should receive appropriate support from nursing staff. |
Evidence that the findings of my investigation have been fed back to relevant staff in a supportive manner for reflection and learning. Evidence staff members are aware of formulary products for skin damage, their use and contraindications. Evidence the Board have in place a process for assessing whether pressure assist equipment is needed and that this equipment is available for use when required. By: 23 September 2025 If any gaps in care are identified by the audit (in recommendation 4), evidence that these have been addressed to avoid a similar situation happening again. By: 23 January 2026 |
In providing information in response to enquiries made by my complaints reviewer, the Board were asked to provide both clinical notes from admissions to hospital and the district nursing notes prior to admission to hospital. The district nursing notes were not provided in response to this initial enquiry.
When my complaints reviewer contacted the Board to notify them that the complaint would be investigated, they made a further specific request for district nursing notes to be provided. In response the Board provided a copy of the written ‘house’ notes from A’s home. There was no indication that any other notes were available.
Very late in my investigation the Board disclosed that there were further electronic district nursing notes held within their TRAK system. Once aware that there were further electronic notes available, my complaints reviewer requested that these be shared with us.
When we make enquiries to organisations for records relating to a complaint, and particularly in the case of medical records, we ask that all the relevant records relating to the complaint be provided. In this case, both the written and electronic district nursing notes should have been provided in response to our initial request for medical records. Not doing so extended the time taken for me to complete my investigation.
I expect all Boards to provide all the relevant information in response to my office’s initial request and I urge the Board to ensure this happens going forwards.
The complainant (C, an advocate) complained to me on behalf of A’s family about the standard of medical care and treatment provided to A by Lanarkshire NHS Board (the Board) when A was diagnosed with a bleed in the brain.
A had undergone surgery for cancer and while recovering at home, they began to experience symptoms that were later found to be due to a subarachnoid haemorrhage (a type of bleed in the brain). A was admitted to hospital and medical staff sought advice from a neurosurgical team at another health board. That team advised that A should have a stroke review, a CT angiogram (a type of x-ray used to examine blood vessels) and an MRI (a type of scan used to see inside the body) to find out the cause of the bleeding.
A had the CT angiogram but did not have an MRI and was discharged home after two days with a severe headache. A was readmitted the following day when their condition deteriorated. After emergency surgery at another hospital, and a long hospital admission, A died.
The Board said in their response to C that, overall, they considered A’s care was appropriate; they had sought and followed specialist neurosurgical advice. On the day of discharge, A was clinically stable and medical staff contacted the neurosurgical team who advised that no follow-up was necessary and to discharge A home.
C complained to me that A should not have been discharged from hospital when medical staff knew A had a subarachnoid haemorrhage and a severe headache.
During my investigation I sought independent advice from a Consultant Physician in Acute Medicine. Having considered and accepted the advice I received, I found that:
Taking all of the above into account, I upheld C’s complaint about the standard of medical care and treatment provided to A.
Having considered the Board’s complaint file and the evidence from the clinical records, I also found that the Board’s complaint handling was unreasonable and made recommendations to address this, in doing so I drew attention to my concern that my office had made a number of similar findings about the Board’s complaint handling in previous investigation cases.
What we are asking the Board to do for C:
| Rec. number | What we found | What the organisation should do | What we need to see |
|---|---|---|---|
| 1. |
Under complaint point (a) I found that the standard of medical care and treatment was unreasonable in that before discharging A the Board failed to:
Under complaint point (b) I found that complaint handling was unreasonable in that there was a failure to:
|
Apologise to C for the failings identified in this investigation in relation to the standard of medical care and treatment and complaint handling. The apology should meet the standards set out in the SPSO guidelines on apology available at www.spso.org.uk/meaningful-apologies. |
A copy or record of the apology. By: 23 August 2025 |
We are asking the Board to improve the way they do things:
| Rec. number | What we found | Outcome needed | What we need to see |
|---|---|---|---|
| 2. |
Under complaint point (a) I found that the standard of medical care and treatment was unreasonable in that before discharging A the Board failed to:
|
Patients who suffer from an SAH should receive care and treatment that is line with the relevant guidelines and advice from specialist teams. If departing from relevant guidelines and/or specialist advice, this should be clearly documented including the reasons for doing so. Reviews carried out (e.g. stroke review) should be fully documented. |
Evidence that the findings of my investigation have been fed back to the relevant clinical staff, in a supportive manner, for reflection and learning. By: 23 August 2025 Evidence that the Board have reviewed their systems to ensure the relevant guidelines for treating SAH are embedded in working practices and that reviews carried out are fully documented. Evidence that the Board have monitored awareness of and compliance with the relevant guidelines in relation to this. For example, by the carrying out of an audit, and identifying and addressing training needs. By: 23 October 2025 |
We are asking the Board to do to improve their complaints handling:
| Rec. number | What we found | Outcome needed | What we need to see |
|---|---|---|---|
| 3. |
Under complaint point (b) I found that complaint handling was unreasonable in that there was a failure to:
|
Complaints should be investigated fairly and fully and in line with the requirements of the NHS Model Complaints Handling Procedure. Complaint responses should be accurate, complete and address all the points raised in line with the NHS Model Complaints Handling Procedure. All relevant information in relation to an SPSO investigation should be provided at the outset of our enquiries. We offer SPSO accredited Complaints Handling training. Details and registration forms for our online self-guided Good Complaints Handling course (Stage 1) and our online trainer-led Complaints Investigation Skills course (Stage 2) are available at https://www.spso.org.uk/training-courses. |
Evidence that the findings of my investigation have been fed back to the staff involved, in a supportive manner, for reflection and learning. By: 23 August 2025 Evidence that the Board have reviewed their procedures for complaints handling to ensure that all relevant evidence is obtained (including from other organisations) and evaluated during the investigation. Evidence that the training needs for complaint handling staff have been assessed and that relevant staff have access to online training and other tools to improve complaint handling and their approach to our investigations and findings. Evidence that the Board have monitored compliance with the Model Complaints Handling Procedure and SPSO legislation, for example, by the carrying out of an audit. By: 23 October 2025 |
My investigation has found that the standard of communication between clinicians may have been a contributory factor to why the planned MRI was not undertaken. I encourage the Board to reflect on this with clinicians.
In this month’s edition of the Ombudsman’s findings, we highlight our recent investigation reports.
During June we