Scottish Welfare Fund update - February 2025
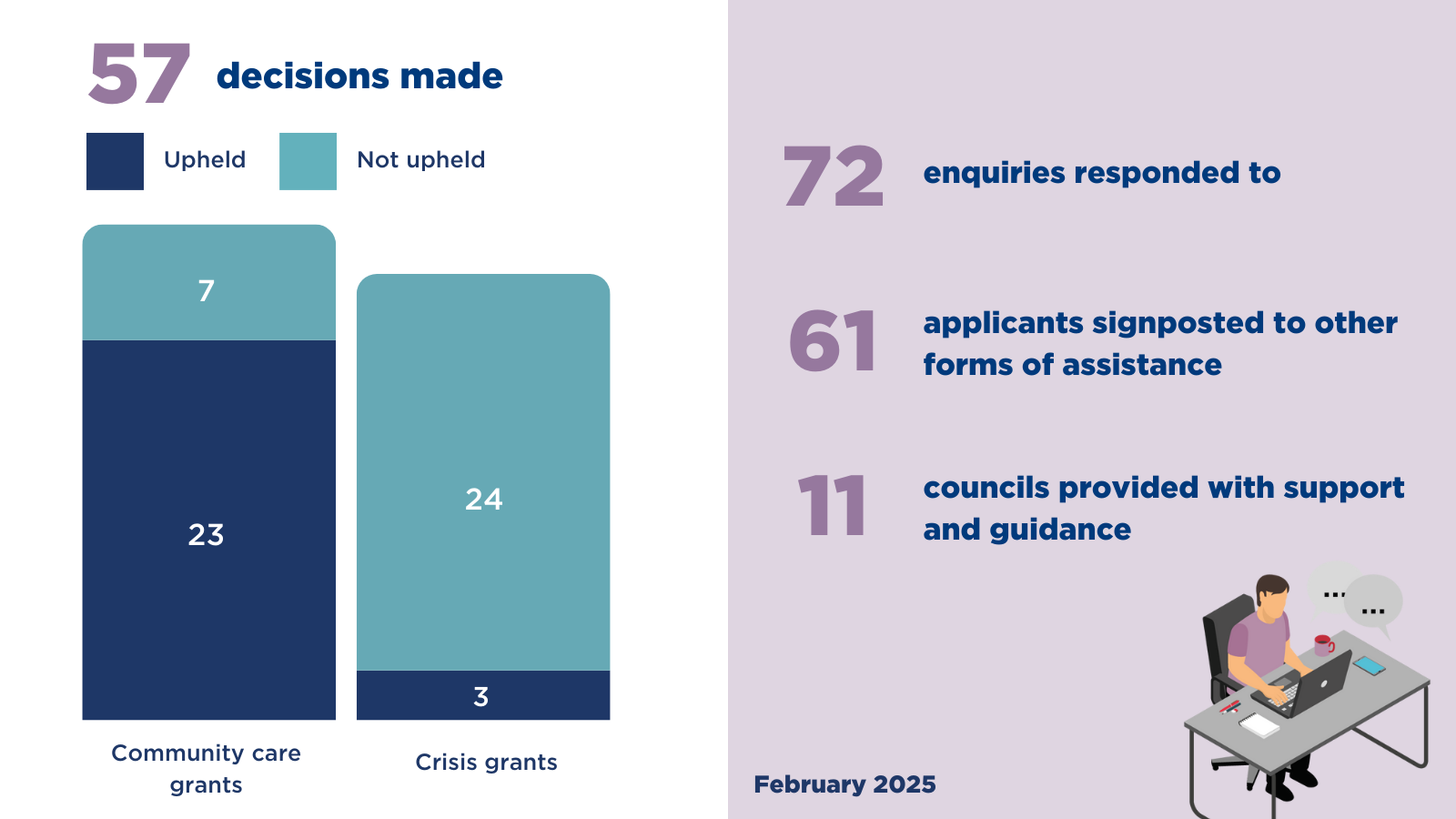
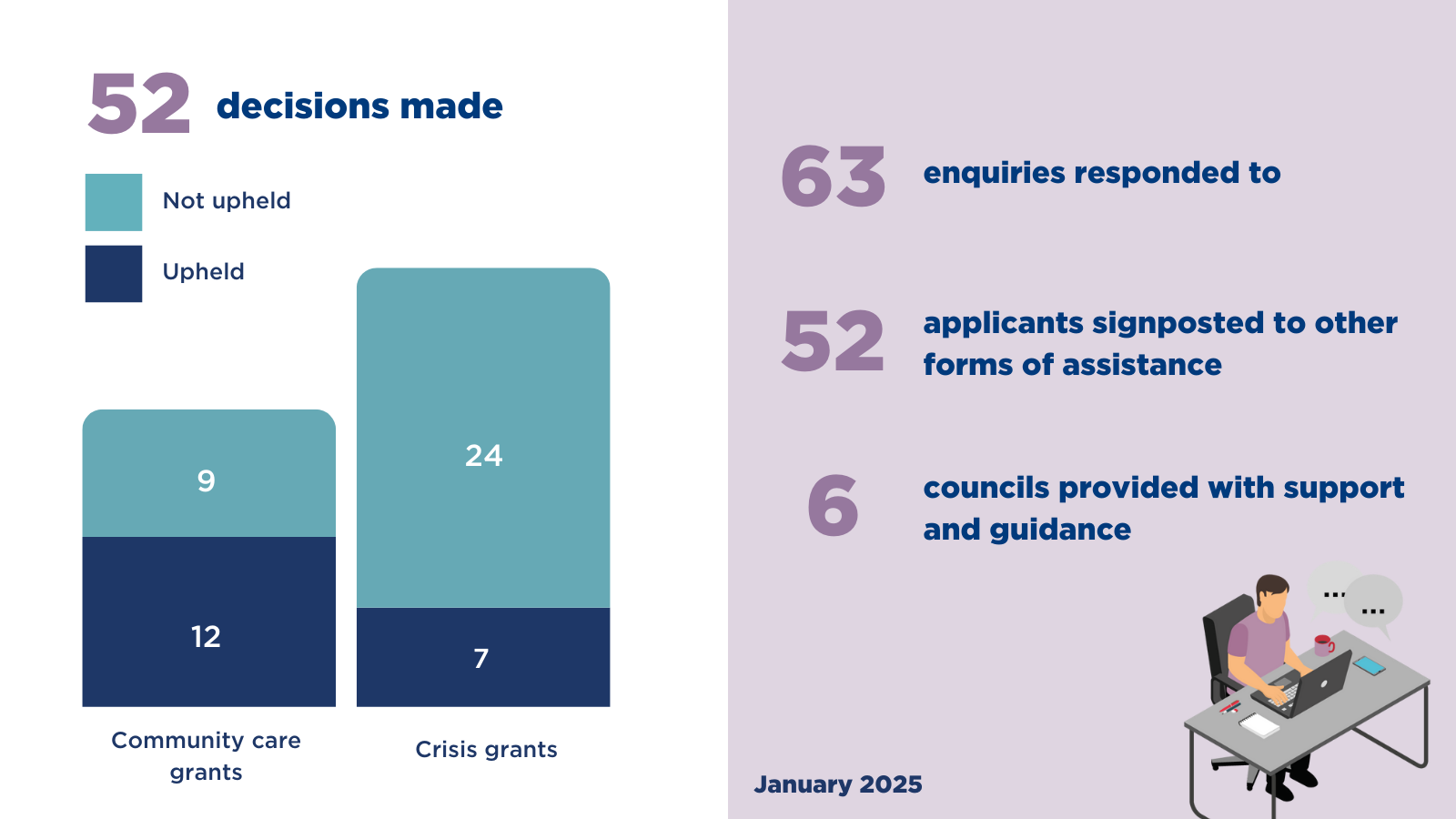
During January, our SWF team
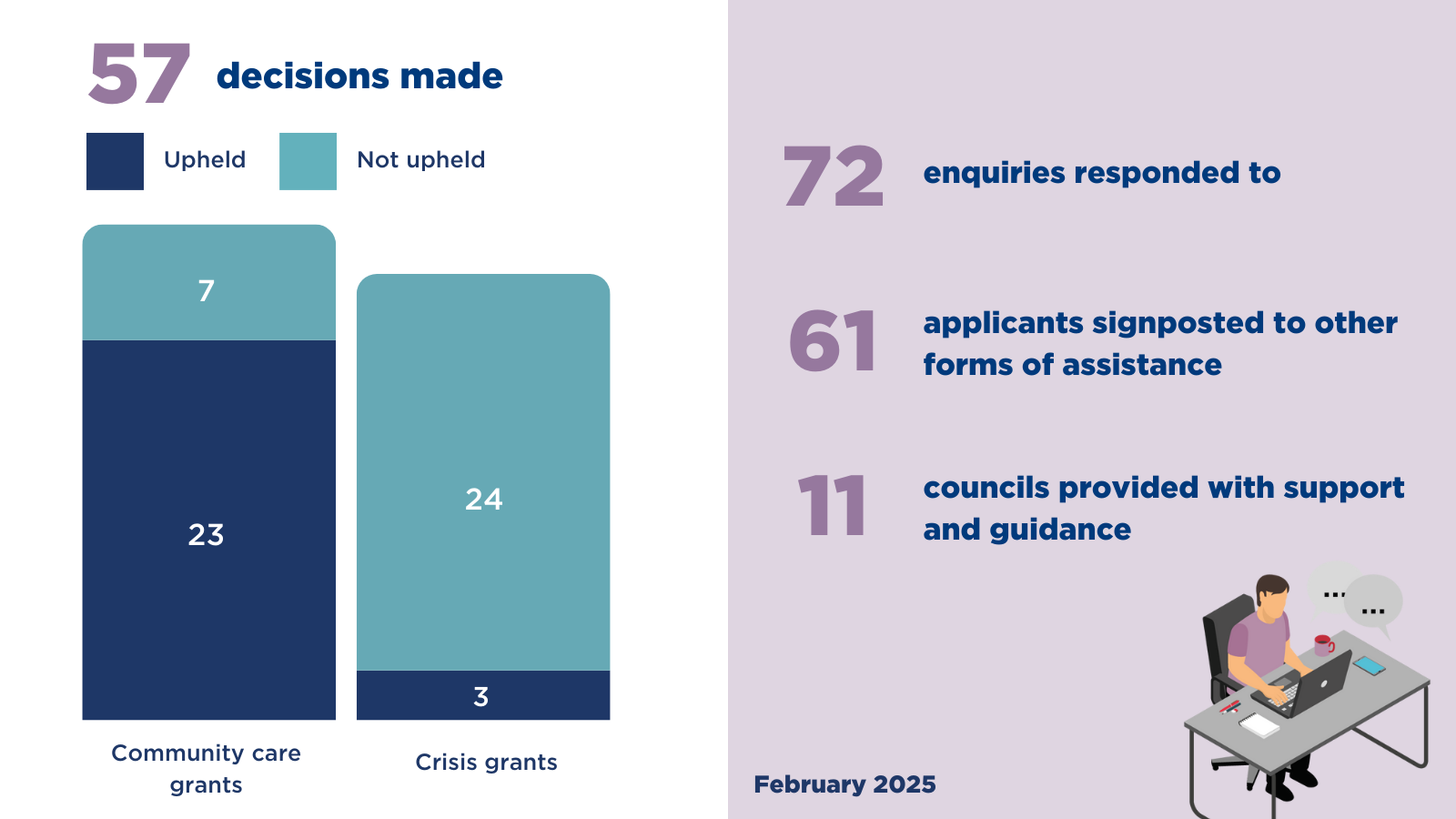
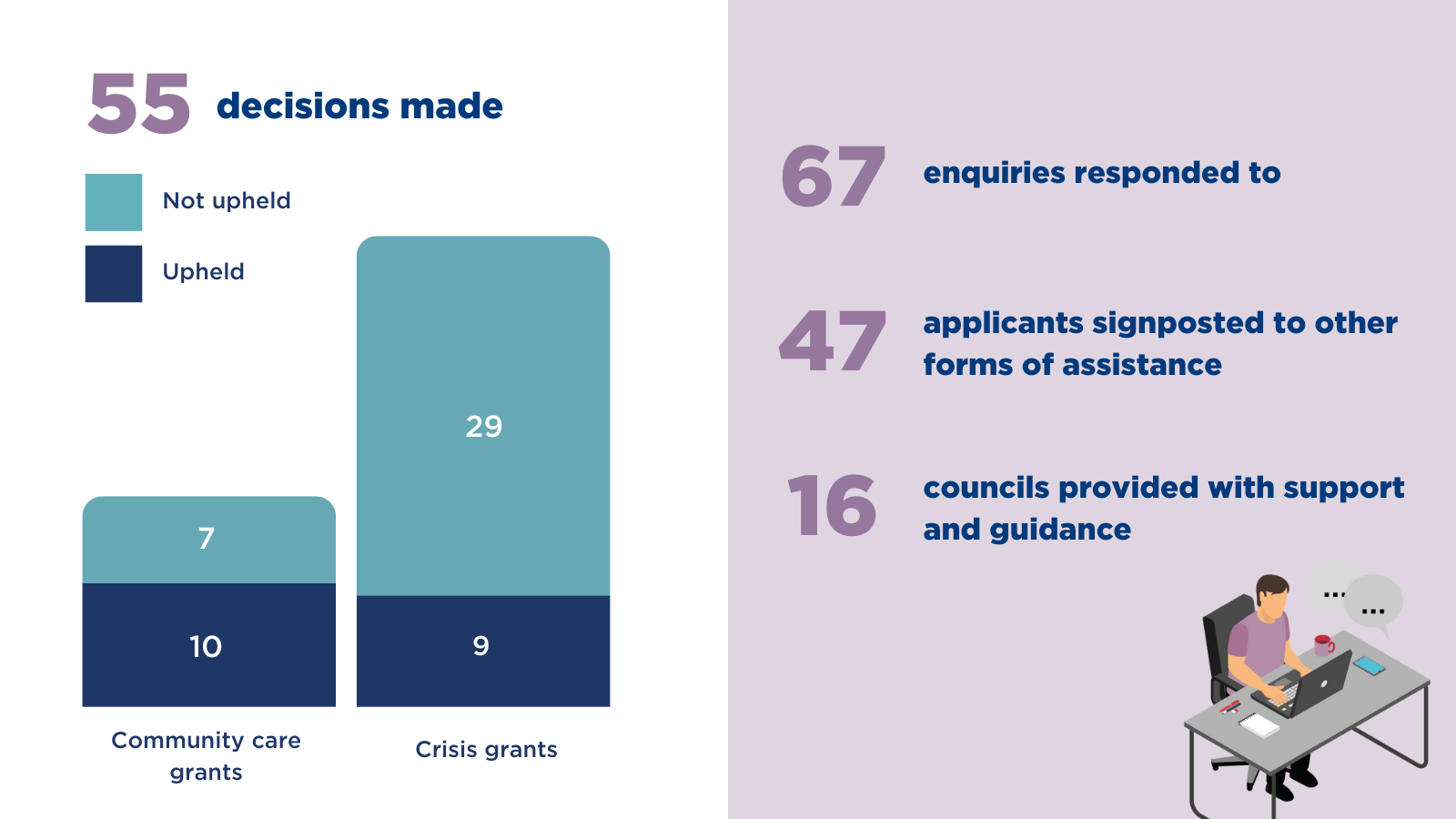
During January, our SWF team
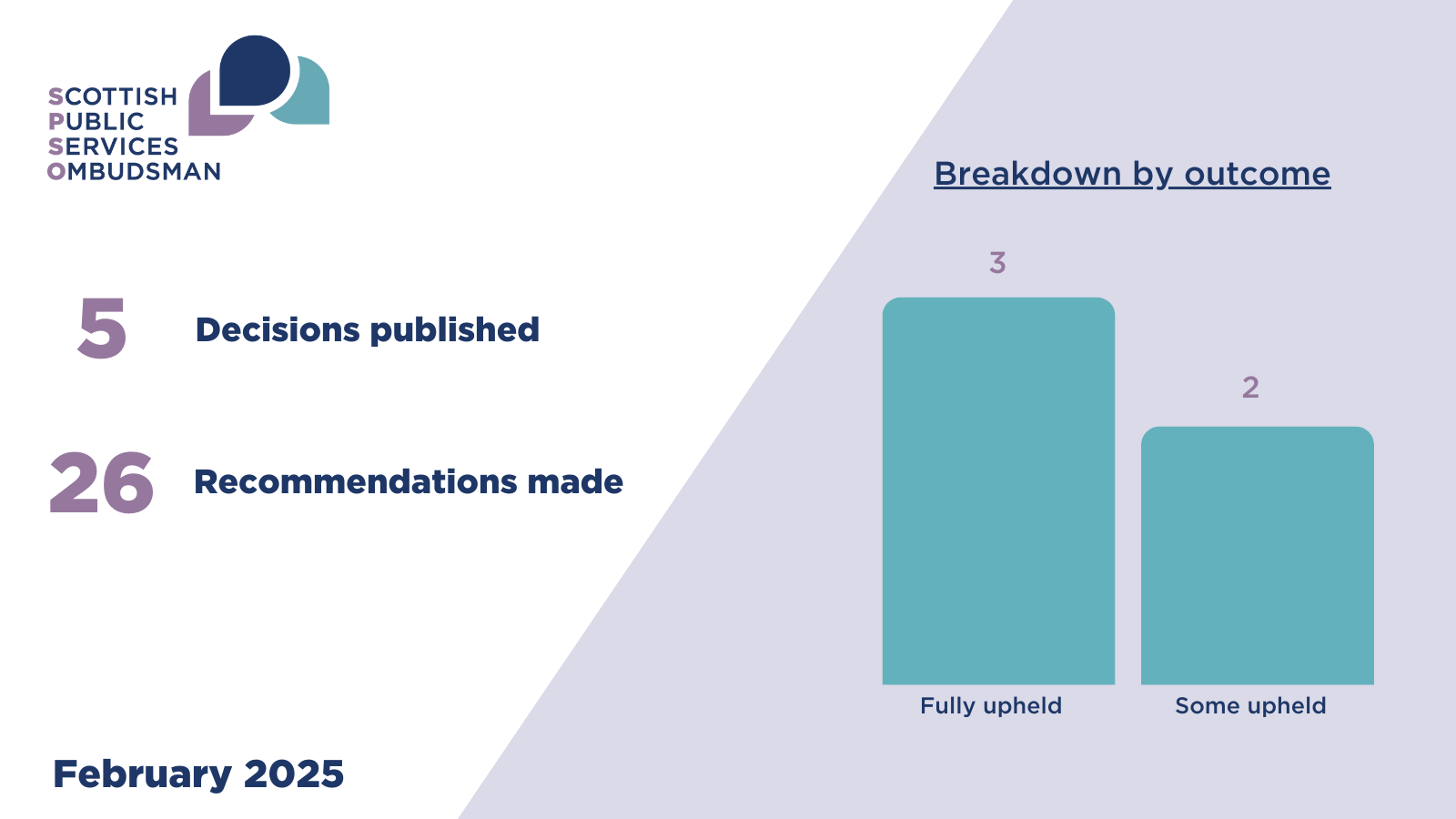
In this month’s edition of the Ombudsman’s findings, we highlight our recent investigation reports.
This month we published decision reports from five complaints investigated by the Ombudsman. All five were about health services. The outcome of these five complaints were
The complainant (C) complained to my office about the care and treatment provided to their late grandparent (A) by Lanarkshire NHS Board (the Board).
A arrived at the Emergency Department of University Hospital Monklands by ambulance in the afternoon of 11 June 2022 and was admitted to hospital in the early hours of 12 June 2022.
While in hospital, A’s condition deteriorated. Over the course of the evening of 12 June 2022, A became seriously unwell. A vomited, developed abdominal pain, and had a distended abdomen. A received abdominal x-rays and input from the surgical team, and staff attempted to stabilise A.
A small bowel obstruction (narrowing or blockage in the bowel, which usually requires urgent treatment) was identified in the early hours of 13 June 2022. Sadly, A died a short time later.
C complained to me (having been though the Board’s complaint process) about the events preceding A’s death. In particular, C complained about events relating to the assessment of A on admission and that communication with A’s family prior to A’s death was unreasonable.
The Board reviewed this case again after receiving notification of my investigation and identified some areas for improvement. They determined that further investigation through a Significant Adverse Event Review (SAER) was not required.
During my investigation I took independent advice from a Consultant in Acute and General Medicine. Having considered and accepted the advice I received, I found that:
Care and treatment
Taking all of the above into account, I upheld C’s complaint about A’s care and treatment. I did not uphold C’s complaint about the Board’s communication.
I was also critical that a SAER was not held in this case given it related to an unexpected death and given the Board’s review had identified three specific points where consideration should be given to escalating to a SAER.
Finally, I found the Board’s handling of C’s complaint was unreasonable.
Further comment
It is of concern to me that I have made similar findings regarding Health Boards not carrying out adverse event reviews in other recent public reports (case references 202100979; 202209575; 202100560; 202101928; 202105840; 202200588). I intend to write to the Scottish Government and Health Improvement Scotland to draw their attention to the findings and recommendations I have made in relation to adverse event reviews in recent cases, including this one.
The Ombudsman’s recommendations are set out below:
What we are asking the Board to do for C:
|
Rec number |
What we found |
What the organisation should do |
What we need to see |
|---|---|---|---|
|
1. |
Under complaint point a) I found the Board’s care and treatment fell below a reasonable standard. In particular I found the Board should have:
|
Apologise to C for the failings identified in this investigation. The apology should meet the standards set out in the SPSO guidelines on apology available at www.spso.org.uk/meaningful-apologies |
A copy or record of the apology. By: 19 March 2025 |
We are asking the Board to improve the way they do things:
|
Rec number |
What we found |
Outcome needed |
What we need to see |
|---|---|---|---|
|
2. |
Under complaint point a) I found the Board’s care and treatment fell below a reasonable standard. In particular I found the Board should have:
|
Patients presenting with diarrhoea and vomiting should have their symptoms fully assessed and be appropriately examined in a timely manner in line with relevant guidance. |
Evidence the findings of my investigation has been shared with relevant staff in a supportive manner for reflection and learning. By: 16 April 2025 Evidence that the Board have reviewed their guidance for the screening of C. diff to ensure it is in line with national guidance in relation to the carrying out of an x-ray with details provided of any changes and how this will be disseminated to staff. Evidence that the Board have reviewed their guidance for clinical staff in the medical assessment unit in relation to the carrying out of abdominal examinations and x-rays and the recording of findings with details provided of any changes and how this will be disseminated to staff. By: 16 May 2025
|
|
3. |
The Board’s review into A’s case following notification of my investigation did not identify all of the significant failings in care and areas for improvement, including that this was a potentially preventable death. The Board did not appropriately consider carrying out a SAER. |
Reviews into patient care should be undertaken at the right time, identify failings and good practice, and findings and recommendations are followed up, to demonstrate learning. Where adverse event(s) occur a significant adverse event review should be held in line with the Board’s protocols and national guidance to ensure there is appropriate learning and service improvements that enhance patient safety. |
Evidence the findings of my investigation has been shared with relevant staff in a supportive manner for reflection and learning. By: 16 April 2025 Evidence that the Board’s systems for carrying out significant adverse event reviews have been reviewed to ensure they are carried out in line with the Board’s protocols and national guidance. By: 16 May 2025 |
We are asking the Board to improve their complaints handling:
|
Rec number |
What we found |
Outcome needed |
What we need to see |
|---|---|---|---|
|
4. |
The Board’s complaint handling was unreasonable. In particular I found the Board should have:
|
Complaints should be investigated and responded to in accordance with the Board’s complaint handling procedure and the NHS Model Complaints Handling Procedure. Complaints investigators should fully investigate and address the key issues raised, identify and action appropriate learning. |
Evidence that these findings have been fed back to relevant staff in a supportive manner that encourages learning, including reference to what that learning is (for example, a record of a meeting with staff; or feedback given at one-to-one sessions). By: 16 April 2025 |
The Board told me they had already taken action to address the issues and provided me with an action log which I am satisfied are reasonable. I will ask them to confirm that all actions are now complete and for an explanation about how they will assess their effectiveness going forward. (By 16 April 2025)
In the advice I took (and accepted), the Adviser said that:
I am drawing these points to the Board’s attention and encourage them to consider and reflect on them, and whether there is scope for further learning from them.
The complainant (C) complained to my office about the treatment provided to their late parent (A) by Greater Glasgow and Clyde NHS Board - Acute Services Division (the Board).
A had a number of pre-existing health conditions and had previously had a laryngectomy (the surgical removal of the larynx (voice box) which disconnects the upper airway (nose and mouth) from the lungs). A had a laryngectomy ‘larytube’ stoma and cannula in situ (where the trachea (windpipe) is cut and then the open end is stitched onto the front of the neck).
On 20 April 2021, A had a fall at home and was taken to the Emergency Department (ED) at Glasgow Royal Infirmary (the hospital) via ambulance. A was admitted to the Acute Medical Receiving Unit (AMRU). A Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) Order was put in place (meaning a patient does not receive resuscitation where their heart stops beating or their breathing stops).
On 21 April 2021, A indicated that they felt that their larytube was blocked. A student nurse provided laryngectomy care to A and was unable to replace the larytube. A experienced respiratory arrest (where breathing stops) followed by a cardiac arrest (where the heart stops beating) and sadly died.
The Board carried out a Significant Adverse Event Review (SAER). In their SAER, and their written response to C’s complaint, the Board’s overall conclusion was that the care provided to A was both appropriate and competent despite some failings having been identified.
C complained to my office about aspects of A’s laryngectomy care, including the decision to put a DNACPR Order in place and the conclusions reached by the SAER investigation.
During my investigation I sought independent advice from Consultant Physician in Acute Medicine and a Consultant Ear, Nose and Throat (ENT) Surgeon. Having considered and accepted the advice I received, I found that:
Taking all of the above into account, I upheld C’s complaints.
Redress and Recommendations
The Ombudsman’s recommendations are set out below:
What we are asking Greater Glasgow and Clyde NHS Board - Acute Services Division to do for the complainant:
|
Rec. number |
What we found |
What the organisation should do |
What we need to see |
|---|---|---|---|
|
1. |
Under complaint point (a) I found:
Under complaint point (b) I found:
|
Apologise to C and her family for:
The apology should be specific and meet the standards set out in the SPSO guidelines on apology available at www.spso.org.uk/information-leaflets |
A copy or record of the apology. By: 19 March 2025 |
We are asking Greater Glasgow and Clyde NHS Board - Acute Services Division to improve the way they do things:
|
Rec. number |
What we found |
Outcome needed |
What we need to see |
|---|---|---|---|
|
2. |
Under complaint point (a) I found it was unreasonable that A did not receive adequate humidification. |
Patients with laryngectomies should receive appropriate humidification as set out in The National Tracheostomy Safety Programme (NTSP) guidelines. |
Evidence that:
By: 19 August 2025 |
|
3. |
Under complaint point (a) I found it was unreasonable that airway help was not sought immediately when the laryngectomy cannula could not be reinserted. |
Where there is a difficulty reinserting laryngectomy cannulas, airway help should be sought without delay. |
|
|
4. |
Under complaint point (a) I found it was unreasonable that ventilation/ resuscitation was not attempted in the circumstances of A’s case. |
Decisions in relation to ventilation/ resuscitation when a DNACPR is in place should be taken in line with relevant national guidance. Where a decision is taken not to follow relevant national guidance this decision, and the reasons for it, should be clearly recorded. |
|
|
5. |
Under complaint point (b) I found that there was a failure to activate the duty of candour process in this case. |
When an incident occurs that falls within the duty of candour legislation, the Board’s Duty of Candour processes should be activated without delay. |
Evidence that the Board have reviewed their Duty of Candour processes, including their process for identifying and activating the process. By: 19 May 2025 |
|
6. |
Under complaint point (b) I found that there was a failure to undertake a reasonable Significant Adverse Event Review that identified key learning and improvements. |
Local and Significant adverse event reviews should be reflective and learning processes that ensure failings are identified and any appropriate learning and improvement taken forward. Adverse event reviews should be held in line with relevant guidance. |
Evidence that the Board have reviewed their process for carrying out adverse event reviews to ensure these reviews properly investigate, identify learnings, and develop system improvements to prevent similar incidents occurring. By: 19 May 2025 |
|
7. |
Under complaint point (b) I found that the Board unreasonably recorded a conclusion of Code 2 (Issues identified but they did not contribute to the event) on the SAER when a conclusion of Code 3 (Issues identified which may have caused or contributed to the event) would have been more appropriate. |
Conclusion codes on adverse event reviews should reflect the findings. |
Evidence that the Board have noted the incorrect conclusion code on the SAER report and have ensured this is a matter of record either by reissuing a revised SAER report, or by issuing an addendum, in line with any relevant Healthcare Improvement Scotland guidance and advice. By: 19 May 2025 |
We are asking Greater Glasgow and Clyde NHS Board - Acute Services Division to improve their complaints handling:
|
Rec. number |
What we found |
Outcome needed |
What we need to see |
|---|---|---|---|
|
8. |
There was a failure to fully investigate and identify the significant failings in this case in accordance with the Board’s complaint handling procedure and the NHS Model Complaints Handling Procedure. There was also a failure to apologise to C as part of the complaint response. |
Complaints should be investigated and responded to in accordance with the Board’s complaint handling procedure and the NHS Model Complaints Handling Procedure. Complaints investigators should fully investigate and address the key issues raised, identify and action appropriate learning and apologise where issues have been identified. |
Evidence that:
By: 19 May 2025 |
Feedback
Response to SPSO investigation
The Board’s response to our enquiries initially provided us with the accounts of different specialists employed by the Board which differed in opinion on some significant points, without providing the Board’s overall view. This resulted in delays to our investigation while we established what the Board’s overall view was. When responding to SPSO enquiries, the Board should ensure that their response reflects the Board’s overall position. I am including this as feedback for the Board to reflect on.
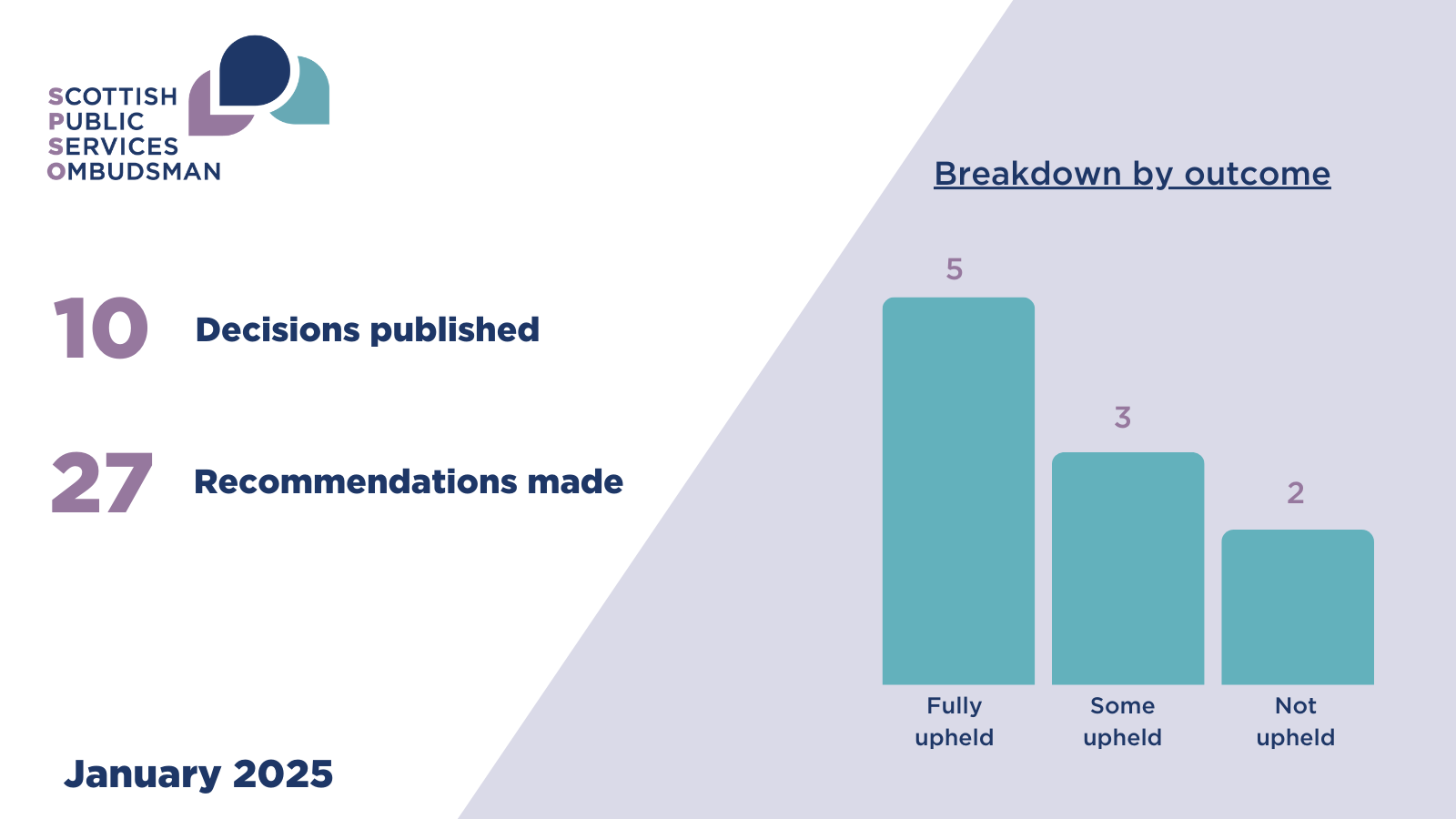
In this month’s edition of the Ombudsman’s findings, we discuss primary care
This month we published decision reports from ten complaints investigated by the Ombudsman. All ten were about health services. The outcome of these ten complaints were
During December our SWF team
The complainant (C) complained to my office about the care and treatment provided to their late adult child (A) by Lothian NHS Board – Acute Division (the Board).
A was in their thirties and suffered from a number of chronic illnesses and very poor health. A had regular admissions to hospital and received treatment from community and district nurses between admissions to hospital.
A was admitted to the Royal Infirmary of Edinburgh (the hospital) on 6 June 2021 with shortness of breath. A’s pre-existing leg wounds were treated in hospital during their admissions. A was discharged home on 24 June 2021. A continued to receive treatment at home from district nurses for their leg wounds.
A’s condition deteriorated and they were admitted to hospital again on 26 August 2021. A’s health continued to deteriorate, and A underwent a right knee amputation on 2 September 2021. A did not make a full recovery following surgery. A remained in hospital and suffered a cardiac arrest on 11 October 2021. Sadly, A died the same day.
C complained that A’s wounds were not appropriately assessed or treated during their admission to hospital, or during the time they were cared for at home.
In their complaint response the Board said that throughout A’s care, where infection was suspected by the district nursing team, appropriate treatment was provided. During the course of treatment at home by district nurses, A’s care plan was reviewed regularly, changes were made to the wound care plan when necessary, dressings were changed when appropriate and a referral made to the tissue viability service.
In response to our enquiries the Board said that there was evidence of good practice during A’s admission to hospital in June 2021 with respect to the management of A’s wounds. The Board acknowledged a wound care chart was not completed on the day of admission, but there were clear entries thereafter evidencing A’s wound care.
With respect to A’s admission to hospital in August 2021, the Board said that A’s wound care was appropriately documented and that available records evidenced appropriate nursing care during A’s admission.
During my investigation I took independent advice from a registered nurse. Having considered and accepted the advice I received, I found that:
Care at home
Care during hospital admissions
Taking all of the above into account, I upheld C’s complaints
What we are asking Lothian NHS Board - Acute Division to do for the complainant
| Rec. number | What we found | What the organisation should do | What we need to see |
|---|---|---|---|
| 1. |
In relation to (a) and (b) I found that:
|
Apologise to C for the failures identified in my decision. The apology should meet the standards set out in the SPSO guidelines on apology available at www.spso.org.uk/information-leaflet. |
A copy or record of the apology. By: 19 February 2025. |
What we are asking Lothian NHS Board - Acute Division to improve the way they do things
| Rec. number | What we found | Outcome needed | What we need to see |
|---|---|---|---|
| 2. | A’s wounds were not appropriately assessed. | Wound assessments for patients should be completed holistically and on a timely basis in line with the patient’s presentation. Assessments should appropriately document the progression/ deterioration of a patient’s wound and prescribe appropriate wound management. |
Evidence that the Board have shared the decision with all staff involved with wound care in a supportive manner for reflection and learning. By: 19 February 2025. Evidence that the Board have reviewed their wound management guidance to ensure it appropriately takes into account relevant national guidance with details of how any changes will be disseminated to staff. Evidence that the Board have reviewed their wound care assessment training for relevant nursing staff in light of the findings of this investigation with details of how it will be rolled out to relevant staff. By: 16 April 2025 |
| 3. |
The frequency of dressing changes was not sufficient to manage A’s wounds. On one occasion hospital at home staff attending A inappropriately left wet and soaked through dressings for district nursing staff to change which was unreasonable, and Dressings applied to A’s wounds were at times not appropriate, contraindicated, or inappropriate to manage their wounds. |
Wound dressings should be changed frequently enough to manage the level of exudate, to prevent ‘strikethrough’ and foul smells. Patients should not be left at home with wet or soaked through dressings unchanged. |
Evidence that the Board have shared the decision with all relevant staff involved with wound care assessment in a supportive manner for reflection and learning. By: 19 February 2025. Evidence that the Board has ensured that staff delivering such services have received the appropriate training and ongoing professional development. This should include details of future plans to either / both provide training now and how expertise will be maintained. By: 16 April 2025 |
| 4. | There was an unreasonable delay in referring A to Tissue Viability Specialists and there was an unreasonable delay in making the referral. |
Where a patient’s wounds deteriorate despite on-going treatment or are non-progressing over a period of time, nursing staff should consider immediate referral for specialist tissue viability assessment. Decisions in relation to referral should be documented and if the need for referral is identified this should be actioned without delay. |
Evidence that The Board have shared the decision with relevant nursing staff involved with wound care in a supportive manner for reflection and learning. By: 19 February 2025. Evidence that the Board have an appropriate referral pathway for specialist wound management and that relevant nursing staff are aware of how to access it to make a referral. By: 16 April 2025. |
| 5. |
Negative Pressure Wound Therapy was inappropriately applied to an actively bleeding wound. Negative Pressure Wound Therapy was also inappropriately applied to a sloughy wound. |
Negative Pressure Wound Therapy should be applied in accordance with manufacturers guidance and in accordance with Board policy and HIS guidance. |
Evidence that the Board have shared the decision with all relevant staff involved in wound management. By: 19 February 2025. Evidence that relevant staff are aware of the Board’s policy on the use of Negative Pressure Wound Therapy and manufacturers guidelines, and that medical staff deemed competent in prescribing/applying Negative Pressure Wound Therapy have received training in its use. By: 16 April 2025 |
The ‘house held’ records which contain the written record of care provided at A’s home have been reported as lost. I encourage the Board to reflect on the circumstances leading to their loss, and whether there is any learning for them in relation to record keeping and records management policies and staff guidance.

Rosemary Agnew, the Scottish Public Services Ombudsman (SPSO) has launched online training to help public service organisations handle complaints from or involving children and young people.
The Scottish Parliament has advertised for a new Scottish Public Services Ombudsman (SPSO), as the current term comes to an end in April 2025.
The current Ombudsman, Rosemary Agnew, will conclude her term in April after years of dedicated service. Since her appointment, Rosemary has been instrumental in improving complaints handling processes and promoting fairness across Scotland's public services.
During November we responded to