MCHP page draft
Since 2012 the SPSO's Complaints Standards Unit has worked closely with a range of partners and stakeholders to develop and implement Model Complaints Handling Procedures (MCHPs) for each public service sector.
Since 2012 the SPSO's Complaints Standards Unit has worked closely with a range of partners and stakeholders to develop and implement Model Complaints Handling Procedures (MCHPs) for each public service sector.

During June we:

This month we published decision reports from 20 complaints investigated by the Ombudsman. Thirteen of these were about health services, six about local government and one about a water provider. The outcome of these 20 complaints were
The British Sign Language (Scotland) Act 2015 requires certain bodies, including the Scottish Public Services Ombudsman (SPSO), to produce a British Sign Language (BSL) Plan every six years.
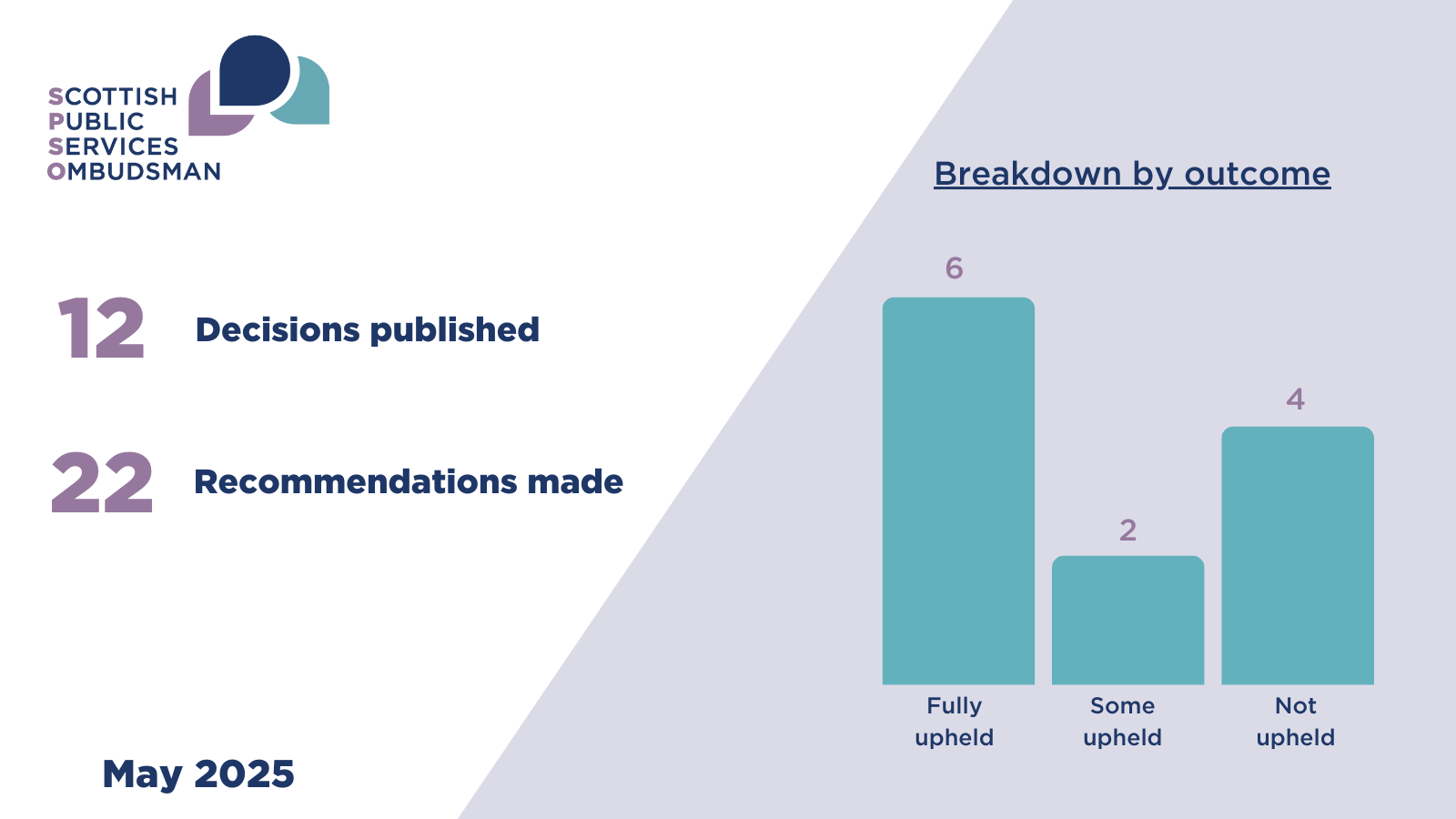
This month we published decision reports from 12 complaints investigated by the Ombudsman. Ten of these were about health services and two about local government. The outcome of these 12 complaints were
We made 22 recommendations to public bodies.
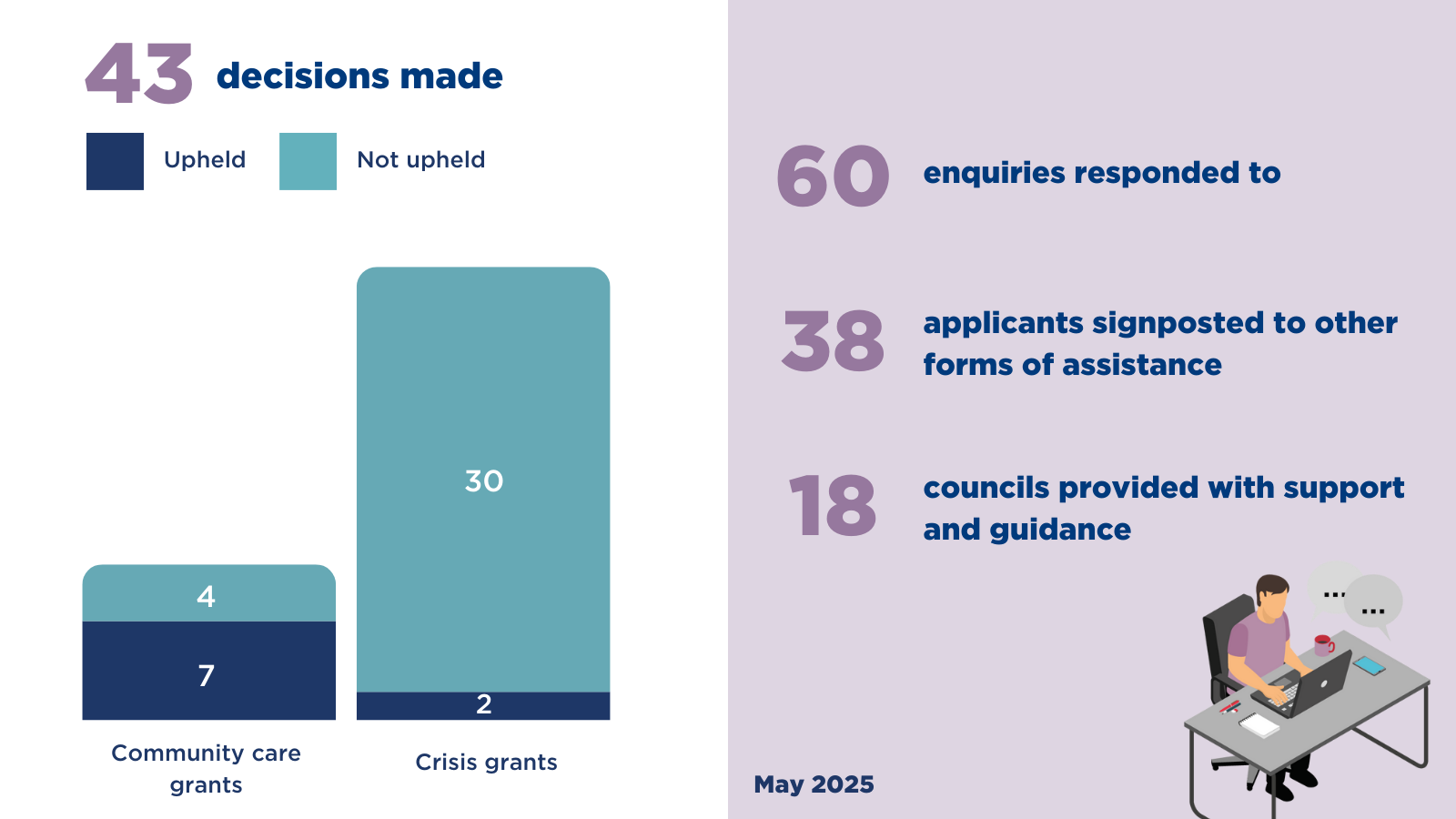
During April we
The complainant (C) complained to my office on behalf of their parent (B) about the response from the Scottish Ambulance Service (the SAS) to requests for an ambulance to attend B’s spouse (A).
A was at home on 6 March 2023 when B and their neighbour (D) called the SAS. In total, three calls were made to the SAS to request an ambulance for A. An ambulance was dispatched in response to the third call; however, A died before its arrival. It was later confirmed that A had suffered a myocardial infarction (a heart attack, when blood flow to the heart is blocked).
C complained to me (having been through the SAS’ complaints process) that the SAS had failed to reasonably respond to the calls made about A. In particular, that Call 1 was inappropriately triaged and there was a failure to re-triage A as an emergency after Call 2 clearly described a significant deterioration. C also complained that the SAS had failed to reasonably respond to their complaint.
In response to C’s complaint the SAS advised that they prioritised the calls using the Medical Priority Dispatch System (MPDS, a computerised system in which a coded response level is determined in response to information provided by the caller). Based on the information input by the call handlers Calls 1 and 2 generated ‘Teal’ responses. Had it been apparent that A was in either cardiac or peri-arrest then call handlers would have documented this, asked further relevant questions and provided further pre-arrival advice and guidance.
During my investigation I took independent advice from a paramedic. Having considered and accepted the advice I received, I found that:
Having listened to the call, I recognise and acknowledge the pressured environment SAS call handlers are in, and that they are required to follow a defined script. Nevertheless, a key symptom was missed, with the key word ‘gasping’ not being picked up. This led to a missed opportunity to identify A’s ineffective breathing. Best practice would have been to have picked it up and acted at this point.
The SAS did not correctly triage Call 2. Information shared about A’s rasping breathing, blue lips, and temperature and clamminess were not acted on, and the call was not coded correctly. This was unreasonable. While it cannot be known what further information would have been provided to the questions that would have been asked if the call had been correctly coded, when cardinal symptoms are mentioned throughout a 999 call it is reasonable to assume that a high category of response would have been provided, which reflected the SAS’ own findings when they audited the call.
The SAS reasonably responded to Call 3.
Taking all of the above into account, I upheld C’s complaint about call handling.
When responding to the first complaint submitted by C, the SAS did not respond to all the key points made. This was unreasonable.
Given the basis of C’s complaint was that A had died as a result of an incorrectly triaged call, it would have been reasonable to expect the calls to have been audited prior to responding to C’s initial complaint.
When C reiterated their questions following receipt of the first complaint response, the SAS provided a more thorough answer. However, they did not disclose in their second response that they had carried out an audit of Call 2 which had identified there was a failing. This was unreasonable, lacked transparency and went against the principles of the duty of candour legislation and good complaint handling.
The SAS should have also considered undertaking a significant adverse event review (SAER). There is no evidence that one was considered which was unreasonable.
Taking all of the above into account, I upheld C’s complaint about the SAS’ handling of the complaint.